
Nutter, a 16-year-old spayed female domestic shorthair, presented to the Emergency Department as a referral for vomiting, lethargy, ataxia, and possible visual impairment. She had been seen at her primary vet earlier that morning, at which time bloodwork was performed and showed an elevated ALT (877), ALP (346), and bilirubin (1.3). Her total T4 hormone was also elevated at 5.1. She was given Cerenia, ondansetron, and subcutaneous fluids prior to referral. Pertinent medical history included recurrent ear infections, chronic right head tilt, and previous bouts of pancreatitis.
On presentation, she was found to have a right head tilt (reportedly chronic), positional rotary nystagmus, aimless pacing and circling to the right, and impaired vision in the right eye with constant bumping into obstacles. She received an abdominal ultrasound, which revealed a fluid-distended stomach. At that time, her problem list included right vestibular dysfunction (thought to be acute on chronic exacerbation), vomiting with gastric distension (ddx gastric atony, IBD, occult foreign body, neoplasia), increased liver enzymes with normal liver and gallbladder, and hyperthyroidism. She was discharged with metoclopramide, Clavamox, Cerenia, and methimazole, with a recheck scheduled for 2 weeks with the Internal Medicine Service.
At Nutter’s recheck, the owner reported that she initially improved but had worsened significantly since the discontinuation of Clavamox. Evaluation by the Neurology Service was recommended. Neurologic exam at that time included the following abnormalities: abnormal, vague mentation; right head tilt, resting vertical nystagmus that worsened with positional changes; depressed menace bilaterally; anisocoria; marked vestibular ataxia; and compulsive approach, giving us a neurolocalization of the brainstem. An MRI was recommended. Given her signalment and history, neoplasia was prioritized, with infectious and inflammatory etiologies considered less likely.
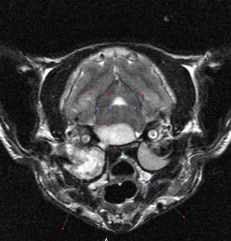
An MRI was performed that day, which showed several abnormalities, including severe chronic right-sided otitis media, interna, and externa, with intracranial extension resulting in a large intracranial extra-axial abscess and increased intracranial pressure.
Nutter was admitted to the hospital and given hypertonic saline to address the intracranial hypertension. She was immediately started on broad-spectrum IV antibiotics, an anti-inflammatory dose of steroids, and GI protectants, in addition to her chronic medications. Her neurologic status was monitored closely. Throughout the course of a 48-hour hospitalization, Nutter steadily showed excellent improvement in her neurologic exam. After 48 hours of antibiotics, she was bright, alert, and responsive with an improved head tilt, resolved nystagmus, resolved anisocoria, and only a very mild vestibular ataxia. Her pacing and compulsive approach had also resolved. She was discharged with Clavamox, pradofloxacin, and prednisolone and continued on her chronic medications.
At the 2-week recheck, Nutter showed only a mild right head tilt with no other neurologic abnormalities. She was continued long-term on her antibiotic regimen at that time and continues to do well almost 1 year later!
